Thrombolysis in Very Minor Ischemic Stroke (NIHSS=0 or 1)
Thorleif Etgen
1Department of Neurology, kbo-Inn- Salzach-Klinikum, Wasserburg am Inn, Germany
2Department of Psychiatry and Psychotherapy, Technische Universität München, Germany
- *Corresponding Author:
- Thorleif Etgen
Department of Neurology, kbo-Inn-Salzach- Klinikum Gabersee 7 D- 83512 Wasserburg am Inn, Germany.
Tel: ++49-8071-71-250
Fax: ++49-8071-71-253
E-mail: thorleif.etgen@kbo.de
Received Date: June 27, 2016; Accepted Date: September 28, 2016; Published Date: October 04, 2016
Citation: Etgen T. Thrombolysis in Very Minor Ischemic Stroke (NIHSS=0 or 1) . Stroke Res Ther. 2016, 1:1.
Abstract
Thrombolysis in Very Minor Ischemic Stroke (NIHSS=0 or 1)
Background: Introduction: Intravenous thrombolysis (IVT) in minor ischemic stroke is controversial and often a minimum score of National Institute of Health Stroke Scale (NIHSS) is recommended for thrombolysis. Clinical characteristics, safety and outcome of very minor ischemic stroke (VMIS) treated by IVT were assessed.
Methods: Data of all patients treated with IVT during the last 5 years were extracted from a prospectively collected database. VMIS was defined as NIHSS=0 or 1 on admission. Baseline demographic data, symptoms, clinical and imaging findings, and outcome of VMIS patients were analysed.
Results: From 2010 to 2014, in total 477 patients were treated with IVT which included 12 VMIS (2.5%) patients. No complication or intracerebral haemorrhage occurred in the VMIS group. Median Rankin scale among VIMS patients improved from 4 at admission to 0 at discharge. Main symptoms of verified VMIS patients comprised mild aphasia/dysarthria (n=3) and gait ataxia (n=7), the latter not being registered by NIHSS.
Conclusions: This data add evidence that IVT may be safely performed in VMIS. VMIS incorporates often gait ataxia resulting from brainstem stroke which is not tested using the NIHSS. Thrombolysis decision should also be based on functional disability.
https://betkolikgirisi.com https://betlikeguncel.com https://betparkagiris.com https://bettickett.com https://betturkeyegiris.com https://extrabetgirisi.com https://holiganbeti.com https://ilbete.com https://ikimisligirisi.com https://imajbetegir.com https://jojobeti.com https://kralbetting.com https://mariogiris.com https://marsbahise.com https://meritegiris.com https://milanobeti.com https://piabetegir.com https://redwinegiris.com https://supertotobete.com https://tempobetegir.com
Keywords
Thrombolysis; Minor Stroke; NIHSS; Ataxia
Background
More than half of all ischemic stroke cases have mild symptom severity on initial presentation [1] but these patients are frequently excluded from thrombolytic therapy [2]. However, this denial of intravenous thrombolysis (IVT) remains controversial as minor ischemic stroke patients do not always have a favorable outcome when left untreated [3].
Data on IVT in patients with very minor ischemic stroke (VMIS) as defined by National Institute of Health Stroke Scale (NIHSS) score=0 or 1are even more limited. So far, only three studies have reported data on VMIS patients [4,5,6].
This study systematically analysed the clinical characteristics, safety and outcome of VMIS patients treated by IVT in a community-based hospital.
Methods
Data of all consecutive stroke patients with IVT admitted to the stroke unit at Klinikum Traunstein, Bavaria, Germany during the period 2010 to 2014 were prospectively recorded at the time of admission of patients. Klinikum Traunstein is a community hospital in a rural area of southeast Bavaria and takes care for approximately 200,000 people [7]. Being a cohort study using a regularly approved therapy and performing all procedures in accordance with institutional guidelines, no specific approval by local ethics committee was required.
Baseline demographic data, symptoms, clinical and imaging findings, and outcome were assessed. Symptomatic intracerebral haemorrhage (sICH) was defined as any haemorrhage type on the post-treatment imaging scan, combined with a neurological deterioration of 4 points or more on the NIHSS from baseline, or from the lowest NIHSS value between baseline and 24 h, or leading to death [8]. Statistical analysis was performed using Statistical Package for the Social Sciences software (SPSS Version 23, Chicago, IL, USA).
Results
During the five-year-period 2010 to 2014, altogether 477 stroke patients received IVT which included 12 (2.5%) patients with VMIS. The yearly number of stroke patients with IVT rose from 64 in the year 2010 to 123 in 2014. With increasing number of thrombolysis patients, minimum and maximum NIHSS of stroke patients changed from 1 (in 2010) to 0 (in 2014) and from 25 (in 2010) to 30 (in 2014), correspondingly.
Details of these 12 VMIS patients are presented in Table 1, median age was 63 years. No complications like angioedema, any haemorrhage including intracerebral haemorrhage occurred. Median Rankin scale improved from 4 at admission to 0 at discharge. After completed diagnostic work-up, in two patients the initially suspected diagnosis of ischemic stroke could not be confirmed. The first of these “stroke mimics” had viral encephalitis and the second stroke mimic suffered from a complex partial seizure. Excluding these two stroke mimics, the main presenting symptoms of the remaining 10 verified VMIS patients comprised gait ataxia (n=7) and mild aphasia/dysarthria (n=3).
| Patient | Sex, Age | Leading symptoms | NIHSS | RS on admission | RS on discharge | Infarct localization | Infarct etiology |
|---|---|---|---|---|---|---|---|
| 1 | m, 71 | gait ataxia, diplopia | 0 | 4 | 0 | brainstem | microangiopathy |
| 2 | f, 39 | gait ataxia, facial hypaesthesia | 1 | 4 | 0 | brainstem | microangiopathy |
| 3 | f, 63 | mild aphasia | 1 | 2 | 0 | left MCA | intervention |
| 4 | m, 62 | mild aphasia | 1 | 2 | 0 | n/a | encephalitis |
| 5 | m, 59 | gait ataxia, nystagmus, mild dysarthria | 1 | 4 | 0 | right parieto- occipital cortical, left cerebellum | cardiogenic |
| 6 | f, 44 | mild aphasia | 1 | 2 | 0 | left MCA | dissection |
| 7 | m, 65 | mild dysarthria | 1 | 2 | 1 | right MCA | microangiopathy |
| 8 | m, 76 | gait ataxia, diplopia | 1 | 4 | 0 | brainstem | cardiogenic |
| 9 | f, 73 | gait ataxia, dysarthria | 1 | 3 | 0 | n/a | Complex focal seizure |
| 10 | f, 44 | gait ataxia, hypaesthesia | 1 | 4 | 1 | Right MCA | cardiogenic |
| 11 | m, 78 | gait ataxia | 0 | 4 | 0 | Right PCA | cryptogenic |
| 12 | m, 62 | gait ataxia, facial palsy, central nystagmus | 1 | 4 | 1 | brainstem | cardiogenic |
Abbreviations: m=male, f=female, NIHSS=National Institute of Health Stroke Scale on admission, RS=modified Rankin Scale, n/a=not applicable, MCA=middle cerebral artery, PCA=posterior cerebral artery
Table 1: Characteristics of patients presenting with very minor ischemic stroke and treated with thrombolysis.
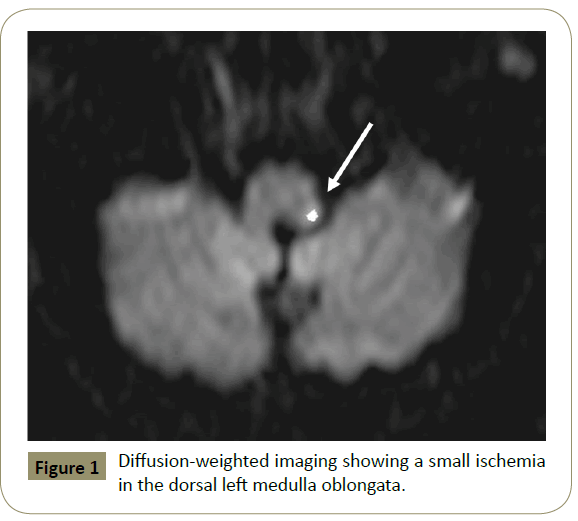
Six of the seven VMIS patients with gait ataxia had vertebrobasilar stroke (4 brainstem, 2 posterior cerebral artery territory). For example, a 39 year old woman (patient 2) presented with acute dizziness which started about 1½ hours earlier. On examination a massive gait ataxia with tendency to fall to the left and hypoesthesia of the left half of the face was noted. Due to the favorable time window and the functionally severe deficit, IVT was performed. Her symptoms regressed completely after IVT. MRI of the brain revealed a small brainstem ischemia (Figure 1).
Discussion
Treatment of patients with minor ischemic stroke is still debatable as the risk-net benefit remains unclear. In an observational registry-based study, standard care with IVT was more effective than not receiving IVT in mild ischemic stroke patients, but there was a statistically nonsignificant risk of symptomatic haemorrhagic transformation [9]. A recent meta-analysis reported an association of good outcome in patients with mild stroke and treatment with IVT without a significant increase in mortality [10]. The analysis of outcomes by clinically important subgroups in the Third International Stroke Trial showed that in those with minor stroke (NIHSS <6), the odds of early death and sICH with tissue-type plasminogen activator (tPA) were at least as great as in patients with more severe stroke. However, for those with milder stroke (NIHSS 0–5) who have a good chance of survival free of dependency without IVT, the 3% risk of sICH (and doubling of the risk of early death with treatment) with thrombolysis has to be considered carefully [11].
Furthermore, the definition of minor ischemic stroke and its applicability for the use of thrombolysis is yet unsettled. An international Delphi study Consensus agreed on a minimal NIHSS score of 2-3 to warrant thrombolysis in stroke patients [6]. On the one hand, a recent pilot survey reported that the majority of clinicians disapproved thrombolysis with an NIHSS score ≤ 1 [2]. On the other hand, another survey of stroke clinicians’ practice patterns revealed that most of the experts do not have an NIHSS threshold below which they would not recommend rtPA; they make this decision based on the perceived disability of the deficit [5]. Finally, a minor or NIHSS score of 0 does not assure the absence of stroke as shown in the present study. Headache, vertigo, nausea, and truncal ataxia constitute alarming symptoms and signs of posterior circulation stroke that are not scored by the NIHSS and could precede a more severe stroke if not addressed early [11].
Data on thrombolysis in patients with very minor ischemic stroke (VMIS) are very limited as only three studies have reported experience with these patients. First, a single centre analysis of off-label use of IVT in acute ischemic stroke found that minor stroke patients (defined by NIHSS<1) had an overall worse outcome compared with the group with on-label use. However, the minor stroke group encompassed only 3 patients without further details [3]. Contrary, the second study compared 1633 patients with mild symptoms (NIHSS ≤5) but without IVT with 158 patients (including 11 patients with NIHSS=0) who received tPA and found that treatment with tPA was associated with an excellent outcome [10]. Finally, a large retrospective analysis of IVT treatment in 5910 mild stroke (NIHSS ≤ 5) patients (including 109 patients with NIHSS=0) yielded that treatment complications were similar across all NIHSS categories. In practice, clinical, functional and imaging considerations are used to decide on the use of thrombolysis in patients with suspected stroke with mild or rapidly improving symptoms. The present study provides further evidence for the safety and efficacy of IVT in patients with minor ischemic strokes using as much as possible, the clinical, brain parenchyma and neurovascular imaging information on their 10 patients.
Despite being a successful and wide-spread tool, the NIHSS has been criticized for some problems. Beyond partially poor reliability, redundancy and complexity, important elements indicating posterior circulation strokes receive no score (e.g. diplopia, dysphagia, gait ataxia, nystagmus) [12]. The newly developed modified National Institutes of Health Stroke Scale (mNIHSS) dropped ataxia as it showed poor reliability so the mNIHSS is still not able to assess brainstem strokes [12]. In contrast, other stroke scores like the Scandinavian Stroke Scale [1] or the European Stroke Score [8] assess gait disorders. The present data show that in all seven patients with gait ataxia NIHSS rating indicated a very mild stroke despite the massive functional disability. Basing the IVT decision solely on NIHSS would have led to a denial of thrombolysis impairing the chance of a good outcome. The importance of a full neurological examination is further underlined by another study of minor stroke patients (NIHSS ≤ 5) not treated with thrombolysis. The results suggested that isolated ataxia should not be simply regarded as a minor symptom given that 23.8% of patients had an unfavourable outcome and 14.3% remained dependent. A substantial proportion of these patients might have a disabling truncal ataxia not reflected in the NIHSS score or a severe brain stem infarction with an initial presenting symptom of ataxia only [13-20].
One major limitation of this present study is the uncontrolled, non-randomized design, which restricts firm conclusions regarding the efficacy of IVT in patients with VMIS. The Study of the Efficacy and Safety of Activase (Alteplase) in Patients with Mild Stroke (PRISMS) will hopefully answer remaining questions [13].
In summary, this study adds evidence that IVT may be safely performed in patients with VMIS who often present with gait ataxia resulting from brainstem stroke. As gait ataxia is not assessed by the NIHSS, thrombolysis decision should be better based on functional disability.
Acknowledgments
None
Conflict of interest
The author has no conflicts of interests.
References
- Reeves M, Khoury J, Alwell K, Moomaw C, Flaherty M, et al. (2013) Distribution of National Institutes of Health stroke scale in the Cincinnati/Northern Kentucky Stroke Study. Stroke 44: 3211-3213.
- Smith EE, Fonarow GC, Reeves MJ, Cox M, Olson DM, et al. (2011) Outcomes in mild or rapidly improving stroke not treated with intravenous recombinant tissue-type plasminogen activator: findings from Get With The Guidelines-Stroke. Stroke 42: 3110-3115.
- Nedeltchev K, Schwegler B, Haefeli T, Brekenfeld C, Gralla J, et al. (2007) Outcome of stroke with mild or rapidly improving symptoms. Stroke 38: 2531-2535.
- Breuer L, Blinzler C, Huttner HB, Kiphuth IC, Schwab S, et al. (2011) Off-label thrombolysis for acute ischemic stroke: rate, clinical outcome and safety are influenced by the definition of 'minor stroke'. Cerebrovasc Dis 32: 177-185.
- Logallo N, Kvistad CE, Naess H, Waje-Andreassen U, Thomassen L (2014) Mild stroke: safety and outcome in patients receiving thrombolysis. ActaNeurolScandSuppl: 37-40.
- Romano JG, Smith EE, Liang L et al. (2015) Outcomes in mild acute ischemic stroke treated with intravenous thrombolysis: a retrospective analysis of the Get With the Guidelines-Stroke registry. JAMA Neurol 72: 423-431.
- Etgen T, Freudenberger T, Schwahn M, Rieder G, Sander D (2011) Multimodal strategy in the successful implementation of a stroke unit in a community hospital. ActaNeurolScand 123: 390-395.
- Wahlgren N, Ahmed N, Dávalos A, Ford GA, Grond M, et al. (2007) Thrombolysis with alteplase for acute ischaemic stroke in the Safe Implementation of Thrombolysis in Stroke-Monitoring Study (SITS-MOST): an observational study. Lancet 369: 275-282.
- Choi JC, Jang MU, Kang K, Park JM, Ko Y, et al. (2015) Comparative effectiveness of standard care with IV thrombolysis versus without IV thrombolysis for mild ischemic stroke. J Am Heart Assoc 4: e001306.
- Yeo LL, Ho R, Paliwal P, Rathakrishnan R, Sharma VK (2014) Intravenously administered tissue plasminogen activator useful in milder strokes? A meta-analysis. J Stroke Cerebrovasc Dis 23: 2156-2162.
- Lindley RI, Wardlaw JM, Whiteley WN, Cohen G, Blackwell L, et al. (2015) Alteplase for acute ischemic stroke: outcomes by clinically important subgroups in the Third International Stroke Trial. Stroke 46: 746-756.
- Dirks M, Niessen LW, Koudstaal PJ, Franke CL, van Oostenbrugge RJ, et al. (2007) Intravenous thrombolysis in acute ischaemic stroke: from trial exclusion criteria to clinical contraindications. An international Delphi study. J NeurolNeurosurg Psychiatry 78: 685-689.
- Balucani C, Bianchi R, Feldmann E, Weedon J, Kolychev D, et al. (2015) To treat or not to treat? Pilot survey for minor and rapidly improving stroke. Stroke 46: 874-876.
- De Los Rios F, Kleindorfer DO, Guzik A, Ortega-Gutierrez S, Sangha N, et al. (2014) Intravenous fibrinolysis eligibility: a survey of stroke clinicians' practice patterns and review of the literature. J Stroke Cerebrovasc Dis 23: 2130-2138.
- Martin-Schild S, Albright KC, Tanksley J, Pandav V, Jones EB, et al. (2011) Zero on the NIHSS does not equal the absence of stroke. Ann Emerg Med 57: 42-45.
- Meyer BC, Lyden PD (2009) The modified National Institutes of Health Stroke Scale: its time has come. Int J Stroke 4: 267-273.
- Scandinavian stroke study group (1985) Multicenter trial of hemodilution in ischemic stroke--background and study protocol. Scandinavian Stroke Study Group. Stroke 16: 885-890.
- Hantson L, De Weerdt W, De Keyser J, Diener HC, Franke C, et al. (1994) The European Stroke Scale. Stroke 25: 2215-2219.
- Park TH, Hong KS, Choi JC, Song P, Lee JS, et al. (2013) Validation of minor stroke definitions for thrombolysis decision making. J Stroke Cerebrovasc Dis 22: 482-490.
- NCT02072226 A Study of the Efficacy and Safety of Activase (Alteplase) in Patients With Mild Stroke (PRISMS).
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences