Clinical Features of Patients Who Come to Hospital at the Super Acute Phase of Stroke
Taizen Nakase and Akifumi Suzuki
Taizen Nakase* and Akifumi Suzuki
Department of Stroke Science, Research Institute for Brain and Blood Vessels-Akita, Japan
- Corresponding Author:
- Taizen Nakase
Department of Stroke Science
Research Institute for Brain and Blood Vessels-Akita, Japan
Tel: +81-18-833-0115
Fax: +81-18-833-2104
E-mail: nakase@akita-noken.jp
Received date: December 21, 2016; Accepted date: January 27, 2017; Published date: February 01, 2017
Citation: Nakase T, Suzuki A. Clinical Features of Patients Who Come to Hospital at the Super Acute Phase of Stroke. Stroke Res Ther. 2016, 1:1.
Abstract
Background: The number of patients who are adopted for acute thrombolytic therapy and/or thrombectomy treatment has not increased for many years. To reveal the clinical reason of this will be important for setting up an effective campaign of stroke awareness.
Methods: Acute stroke patients admitted in hospital within 24 hrs were consecutively screened. The clinical backgrounds were compared between patients for every 6hrs and 6 to 24hrs and also between patients who have taken thrombolysis and/or thrombectomy (interventional therapy) and conventional therapy.
Results: One hundred fifty-four patients and 177 patients were admitted in hospital within 6hrs and 6 to 24 hrs, respectively. There was no difference of the percentage of previous stroke and anti-thrombotic medication between patients admitted within 6 hrs and 6 to 24 hrs. Among patients within 6hrs, the average age was younger and the percentage of diabetes and previous stroke was lower in the interventional therapy group compared with the conventional therapy group (72.2 yo vs. 76.8yo, 7.7% vs. 28.1% and 11.5% vs. 33.6%, respectively).
Conclusions: It can be advised that educating patients by the family doctor might be important for stroke awareness. Moreover, relatively younger healthy people will be the main target for the campaign of stroke awareness.
Keywords
Acute ischemic stroke; Emergency; Time; Stroke campaign; Family doctor
Introduction
More than 10 years past, since the acute thrombolytic therapy using recombinant tissue plasminogen activator (rt-PA) was officially adopted for the acute therapy for ischemic stroke patients in Japan. At the beginning, rt-PA was allowed to administrate within 3 hours after the stroke onset, and the number of rt-PA treated patients were in less than 5% of all acute stroke patients [1,2]. Although the time limit was recently extended to 4.5hrs [3], the number of patients who were treated with rt-PA was not dramatically increased. Recently, it was reported that the rate of thrombolysis in older adults has increased in the United States, from 1.7% to 5.4% (2005-2010 trend) [4]. In mean time, these days, the methods of mechanical thrombectomy have been improving, and this therapy combined with medical management could be safely performed within 8hrs following the stroke onset [5]. Since various therapies have presented as the gospel for acute ischemic stroke patients, it is desirable to increase the number of patients who admitted in hospital at the very early phase of stroke. However, because the initial symptoms of the stroke are various, it would be difficult to decide to go to hospital immediately [6,7]. Actually, many campaign for stroke awareness, including Act FAST (face, arm, speech, time) campaign [8], have been conducted across the globe [9,10], but it’s effect was limited and short [11,12]. Thus far, this study can be a good material for thinking about effective campaign to create awareness on stroke, the clinical distinctive features of acute stroke patients who admitted in the hospital later than 6hrs of stroke onset were investigated by comparing with those of patients who admitted in the hospital within 6hrs and treated with thrombolytic therapy and/or thrombectomy.
Patients and Methods
Following the approval of the ethical committee of Research Institute for Brain and Blood Vessels -Akita, consecutive acute stroke patients admitted in the hospital within 24 hrs following the stroke onset were retrospectively screened between April 2014 and March 2015. All patients consented with written document. Then, 331 acute ischemic stroke patients were enrolled in this study. Diagnosing ischemic stroke was based on the brain magnetic resonance imaging (MRI) or computed tomography (CT) on admission. According to the criteria of the Trial of Org 10172 in the Acute Stroke Treatment classification system [13], stroke subtypes were classified into cardioembolism (CE), large artery atherothrombosis (AT), small vessel occlusion (SV), and other type of infarction (Others). The clinical backgrounds and vascular risks were collected from clinical record. The assessed risk factors were hypertension, dyslipidemia, diabetes mellitus and atrial fibrillation. Previous stroke history and anti-thrombotic medication were also assessed. Patients admitted to the hospital within 6hrs from the stroke onset was classified into the ≤ 6 hrs group. Patients admitted in the hospital between 6 and 24hrs following the stroke onset was classified into the >6 hrs group. Neurologic severity was assessed by the National Institute of Health Stroke Scale (NIHSS) score on admission. The medication was basically adopted by an attending doctor followed by the guidelines [14]. In the ≤ 6 hrs group, if a patient admitted in the hospital within 4.5hrs following the stroke onset and matched to the acute interventional therapy, the thrombolytic therapy using rt-PA (arteplase 0.6 mg/kg) was administrated following the protocol [14]. Moreover, a patient sequentially undertook the mechanical thrombectomy if matched to the criteria, referred to the Japanese Society for Neuroendovascular Therapy. Alternatively, if a patient admitted in the hospital between 4.5 and 6 hrs following the stroke onset, the mechanical thrombectomy was directly considered. The clinical backgrounds were compared between the ≤ 6 hrs group and the >6 hrs group. The clinical features were also compared between patients of the ≤ 6 hrs group with the conventional therapy and those with the interventional therapy.
Statistical Analysis
All data are presented as mean ± standard deviation (SD) for continuous variables and percentage (%) for categorical variables. Clinical characteristics were compared between the >6 hrs group and the ≤ 6 hrs group or the conventional therapy group and the interventional therapy group by the non-parametric one-way analysis of variance (ANOVA) test for continuous variables and by the Pearson χ2 test for categorical variables. All statistical analysis was performed by JMP9 software (SAS Institute Inc., NC).
Results
The numbers of patients were 154 (46.5%) and 177 (53.5%) in the ≤6 hrs group and the >6 hrs group, respectively (Table 1). The age was significantly older to the ≤6 hrs group compared with the >6 hrs group (p=0.001: 76.1yo and 71.5yo, respectively). Regarding the prevalence of risk factors, atrial fibrillation was only observed in significantly higher percentage in the ≤6 hrs group when compared with the >6 hrs group (p=0.017: 29.9% and 18.1%, respectively). There was no significant difference of the frequency of existing previous stroke history and antithrombotic medication between two groups. The ≤ 6 hrs group showed significantly higher percentage of cardioembolism and lower percentage of other type stroke compared with the >6 hrs group (p<0.001: 49.4% vs. 20.3% and 20.1% vs. 39.5%, respectively). NIHSS score was significantly higher in the ≤ 6 hrs group compared with the >6 hrs group (p<0.001: 7.8 and 4.4, respectively).
| >6 hr | =6 hr | p | |
|---|---|---|---|
| N | 177 | 154 | |
| Sex (male/female) | 109/68 | 83/71 | 0.193 |
| Age (ave ± SD) | 71.5 ± 12.1 | 76.1 ± 11.4 | 0.001 |
| Risk factors (n, %) | |||
| Hypertension | 140 (79.1) | 110 (71.4) | 0.136 |
| Dyslipidemia | 88 (49.7) | 66 (42.9) | 0.255 |
| Diabetes | 54 (30.5) | 38 (24.7) | 0.290 |
| Af | 32 (18.1) | 46 (29.9) | 0.017 |
| Prev. stroke | 49 (27.7) | 46 (29.9) | 0.751 |
| Anti-thrombotics | 59 (33.3) | 57 (37.0) | 0.559 |
| Subtypes | |||
| CE | 36 (20.3) | 76 (49.4) | <0.001 |
| AT | 37 (20.9) | 27 (17.5) | 0.525 |
| SV | 34 (19.2) | 19 (12.3) | 0.121 |
| Others | 70 (39.5) | 31 (20.1) | <0.001 |
| NIHSS on admission (ave. ± SD) | 4.4 ± 5.7 | 7.8 ± 8.5 | <0.001 |
Table 1: Clinical characteristics of all patients in each group.
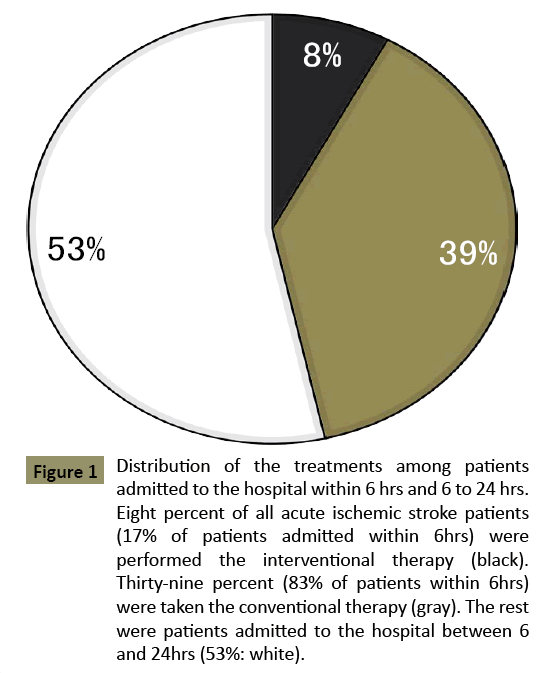
Within the ≤ 6 hrs group, 12 patients were performed only with the thrombolysis therapy, 7 patients were performed only with the mechanical thrombectomy and 7 patients were performed with the thrombolysis and sequential mechanical thrombectomy. As a total, 7.9% of all acute ischemic stroke patients who came to hospital within 24hrs were adopted with interventional therapy (Figure 1). The percentage of female in the interventional therapy was higher than the conservative therapy when compared (Table 2: p=0.041: 50% and 45%, respectively). Patients with the interventional therapy were relatively younger to the conservative therapy (p=0.072: 72.2 yo and 76.8 yo, respectively). Moreover, patients with interventional therapy showed fewer frequency of diabetes and previous stroke history when compared with the conventional therapy (p=0.051: 7.7% vs. 28.1% and p=0.045: 11.5% vs. 33.6%, respectively). The NIHSS score was significantly higher in the interventional therapy when compared with the conventional therapy (p<0.001: 15.6 and 6.2, respectively). The reasons why the interventional therapy was not adopted even though a patient admitted in hospital within 6 hrs were listed in the Table 3. Major reason was mild symptoms (68.0%) followed by large lesion or completed ischemic lesion (11.7%).
| Conservative | Interventional | p | |
|---|---|---|---|
| N | 128 | 26 | |
| Sex (male/female) | 70/58 | 13/13 | 0.049 |
| Age (ave. ± SD) | 76.8 ± 11.2 | 72.2 ± 11.6 | 0.072 |
| Risk factors (n, %) | |||
| Hypertension | 95 (74.2) | 15 (57.7) | 0.144 |
| Dyslipidemia | 56 (43.8) | 10 (38.5) | 0.780 |
| Diabetes | 36 (28.1) | 2 (7.7) | 0.051 |
| Af | 34 (26.6) | 12 (46.2) | 0.080 |
| Prev. stroke | 43 (33.6) | 3 (11.5) | 0.045 |
| Anti-thrombotics | 50 (39.1) | 7 (26.9) | 0.344 |
| Subtypes | |||
| CE | 60 (46.9) | 16 (61.5) | 0.251 |
| AT | 21 (16.4) | 6 (23.1) | 0.594 |
| SV | 18 (14.1) | 1 (3.8) | 0.303 |
| Others | 28 (21.9) | 3 (11.5) | 0.352 |
| NIHSS at admission (ave. ± SD) | 6.2 ± 7.7 | 15.6 ± 8.0 | <0.001 |
Table 2: Clinical characteristics of patients who admitted to hospital within 6 hrs and taken the conservative or interventional therapy.
| Reason | N (%) |
|---|---|
| Mild symptoms (NIHSS=4) | 87 (68.0) |
| Large lesion (=1/3 MCA territory) or Completed ischemic lesion | 15 (11.7) |
| Rapid improvement | 8 (6.3) |
| No major artery lesion in patients of 4.5-6hr | 5 (3.9) |
| Previous ICH | 4 (3.1) |
| Severe general condition | 1 (0.8) |
| Unknown lesion | 1 (0.8) |
Table 3: Reasons why the interventional therapy was not adopted even though a patient admitted in hospital within 6 hrs.
Figure 1: Distribution of the treatments among patients admitted to the hospital within 6 hrs and 6 to 24 hrs. Eight percent of all acute ischemic stroke patients (17% of patients admitted within 6hrs) were performed the interventional therapy (black). Thirty-nine percent (83% of patients within 6hrs) were taken the conventional therapy (gray). The rest were patients admitted to the hospital between 6 and 24hrs (53%: white).
Discussion
Our study clearly demonstrated the distinctive features of patients who came to hospital later than 6hrs, when compared with patients who were suitable for the acute thrombolytic and/ or thrombectomy therapy. Then, it was revealed that patients who were relatively younger healthy people, around 70 yo., should be educated about the emergency of stroke. Moreover, patients who are treated with anti-thrombotic medication must be educated by their family doctors.
At first, this study revealed that there were no difference of the frequency of past stroke history and the percentage of taking antithrombotic medication between the ≤ 6 hrs group and the >6hrs group. This finding suggests that there is a chance to increase the awareness stroke on by the family doctors. Of course, family doctors have to update latest knowledge about stroke, too. Next, the good candidates for the interventional therapy were relatively younger patients with fewer stroke risks. In these cases who did not come to hospital within 6hrs were also relatively young with fewer stroke risks. Therefore, these younger and healthier people, including their relatives, should also become a target of stroke awareness campaign. In the future, conducting a campaign of stroke awareness should be focused on those two groups so that the result will be effective to increase the number of patients who can be adopted to the acute interventional therapy.
Moreover, in this study, we wanted to include the subjects who have taken mechanical thrombectomy along with thrombolytic therapy; the arrival time was set within 6hrs. Then, only atrial fibrillation was observed in significantly higher percentage in the ≤ 6 hrs group compared with the >6 hrs group. This finding corresponded to the fact that stroke subtype of cardioembolism was significantly higher in the ≤ 6 hrs group compared with the >6 hrs group. Actually, cardioembolic stroke has severe neurologic deficits and sudden onset, it is assumed that these patients or bystanders can easily recognize the abnormality and call ambulance in the very early phase. It was reported that cardiogenic embolism was the most abundant subtype of stroke in the patients treated who with thrombolytic therapy [15]. On reflection, it can be said that to be aware of atrial fibrillation is also important to early detection of stroke.
Whereas, for the patients who admitted in the hospital within 6hrs but were not adopted to the interventional therapy, mild neurological deficits was the most frequent reason (68%). It is not a negative result. Since, it can be said that these patients are aware of the stroke symptoms and had known that they immediately have to go to hospital.
This study contains several limitations. Our data was retrospectively collected from one hospital. Therefore, we could not access all acute stroke patients in the area. Moreover, our hospital has a role of the acute stroke center in this area, several stroke patients might be admitted in our hospital. Next, the correcting period was one year and the number of patients, especially patients with interventional therapy, was small. In the future, it needs to conduct a prospective multicenter study.
Conclusion
Educating patients by the family doctor might be effective for stroke awareness. Moreover, relatively healthy younger people will be main target for the stroke awareness campaign.
References
- Hacke W, Kaste M, Bluhmki E, Brozman M, Davalos A, et al (2008) Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Eng J Med 359: 1317-1329.
- Yamamoto Y, Nagakane Y (2015) Percentage of official medications adopted for ischemic stroke treatemnt, and it's annual variation. In: Stroke Data Bank Japan. edn. Edited by Kobayashi S. Tokyo: Nakayama Shoten 88-89.
- Lees KR, Bluhmki E, von Kummer R, Brott TG, Toni D, et al. (2010) Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet 375: 1695-1703.
- George BP, Asemota AO, Dorsey ER, Haider AH, Smart BJ, et al. (2015) United States trends in thrombolysis for older adults with acute ischemic stroke. Clin Neurol Neurosurg 2015: 139:16-23.
- Chen CJ, Ding D, Starke RM, Mehndiratta P, Crowley RW, et al. (2015) Endovascular vs medical management of acute ischemic stroke. Neurology.
- Mackintosh JE, Murtagh MJ, Rodgers H, Thomson RG, Ford GA, et al. (2012) Why people do, or do not, immediately contact emergency medical services following the onset of acute stroke: qualitative interview study. PLoS One 7: e46124.
- Alberts MJ (2012) Improving public education about stroke. Ann N Y Acad Sci 1268: 45-50.
- Wall HK, Beagan BM, O'Neill J, Foell KM, Boddie-Willis CL (2008) Addressing stroke signs and symptoms through public education: the Stroke Heroes Act FAST campaign. Prev Chronic Dis 5: A49.
- Robinson TG, Reid A, Haunton VJ, Wilson A, Naylor AR (2013) The face arm speech test: does it encourage rapid recognition of important stroke warning symptoms? Emerg Med J 30: 467-471.
- Trobbiani K, Freeman K, Arango M, Lalor E, Jenkinson D, et al. (2013) Comparison of stroke warning sign campaigns in Australia, England, and Canada. Int J Stroke 8: 28-31.
- Flynn D, Ford GA, Rodgers H, Price C, Steen N, et al. (2014) A time series evaluation of the FAST National Stroke Awareness Campaign in England. PLoS One 9: e104289.
- Mellon L, Doyle F, Rohde D, Williams D, Hickey A (2015) Stroke warning campaigns: delivering better patient outcomes? A systematic review. Patient Relat Outcome Meas 6: 61-73.
- Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, et al. (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24: 35-41.
- The Joint Committee on Guidlines for the Management of Stroke: Japanese Guidelines for the Management of Stroke 2009.
- Nakagawara J, Minematsu K, Okada Y, Tanahashi N, Nagahiro S, et al. (2010) Thrombolysis with 0.6 mg/kg intravenous alteplase for acute ischemic stroke in routine clinical practice: the Japan post-Marketing Alteplase Registration Study (J-MARS). Stroke 41: 1984-1989.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences