Treatment of Post-Stroke Depression in Young Stroke Survivors
Eun Hyeo Ha and Raymund Gantioque
Eun Hyeo Ha* and Raymund Gantioque
California State University, Los Angeles, USA
- *Corresponding Author:
- Eun Hyeo Ha
California State University, Los Angeles, USA
Tel: 2132005764
E-mail: eha2@calstatela.ed
Received Date: February 08, 2020; Accepted Date: February 19, 2020; Published Date: February 25, 2020
Citation: Ha EH, Gantioque R (2020) Treatment of Post-Stroke Depression in Young Stroke Survivors. Stroke Res Ther Vol.5 No.1. doi: 10.36648/stroke.5.1.1
Copyright: © 2020 Ha EH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Stroke or cerebrovascular accident (CVA) is one of the leading causes of death and long-term disability in the United States. Stroke is most commonly seen in the elderly population. However, studies show that the incidence of this devastating condition is increasing among the younger generation. Potential causes of increased incidences of young people stroke include better diagnostic tests with neuroimaging, increased use of illicit drugs, and increased occurrences of risk factors. Stroke patients are not only affected by long term physical and cognitive disabilities, but also by psychological challenges such as Post-Stroke Depression (PSD). Depression is the most common neuropsychiatric complication of a stroke. However, PSD is often overlooked, and it is an aspect that receives the least attention from clinicians. As a result, there is an increased rate of morbidity and mortality among young stroke victims with depressive symptoms compared to those of the same age without PSD. The purpose of this article is to explore existing knowledge of current guidelines used to treat PSD, specifically in young stroke patients. This is all in an effort to better assist clinicians in treating PSD and in turn improve young patients’ quality of life.
Method: An electronic database search was done through MedLine, PubMed, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Google Scholar. Key words such as “young stroke,” “depression,” and “treatment” were used to gather relevant articles.
Results: Pharmacological therapy with SSRIs and TCAs has been highly successful for PSD in general population. However, no studies were found that specifically address treatment options for young stroke patients.
Conclusion: Clinicians play a crucial role in helping young stroke survivors to recover and possibly resume their previous lives. Therefore, further research is warranted to evaluate the effects of current PSD treatment options that specifically target young stroke population.
https://matadorbet-giris.com https://grandpashabeti.com https://betiste.com https://bahsegelgirisi.com https://klasbahisgirisi.com https://jasminbeti.com https://hepsibahise.com https://dinamobetgirisi.com https://betvolegirisi.com https://betpark-girisi.com https://betlikegiris.com https://betboogirisi.com https://sultanbetegiris.com https://tulipbetgir.com https://padisahbetegir.com https://savoybettinge.com https://goldenbahisegiris.com https://maksibetgirise.com https://fenomengiris.com https://jojobetgiris.xyz https://tarafgiris.com
Keywords
Post-stroke depression; Young stroke; Treatment
Introduction
Stroke is defined as a sudden loss of brain function due to a thrombus, embolus, or hemorrhage [1]. This condition leads to life-changing complications, and it is one of the major causes of death in the United States [2]. Thanks to the advancement of technology and awareness in identifying and treating strokes early, the overall hospitalization rate for stroke patients has been declining [3]. However, the incidences of this disorder have been rising among those who are of younger age [3,4].
Modifiable risk factors for stroke in young patients are similar to those of the elderly. Hypertension, diabetes mellitus, and heart disease are the most common risk factors for older patients. However, the prevalence of these risk factors is different between the two age groups. Smoking (49%), dyslipidemia (46%), and hypertension (36%) were the most frequent risk factors found in 3,944 young stroke patients in Europe [5,6]. When defining what “young stroke” means, studies vary widely and a specific definition of “young stroke” is lacking. However, the majority of studies consider it as patients who are adults of working age, from 18 to 64 year olds [3,7].
Young stroke on the rise
Ramirez et al. [3] assessed the National Inpatient Sample study (the largest inpatient care database in the United States) for hospitalization rate related to stroke from 2000 to 2010 and found that the hospitalization rate for stroke decreased in patients aged 65 to 84. However, there was an increased rate of stroke related hospitalization in patients aged 25 to 44 years (16 to 23 per 100,000) and 45 to 64 years (149 to 156 per 100,000) [3]. Consistent with the previous finding, another study done in Denmark also showed a substantial increased rate of hospitalizations in young adults due to ischemic stroke [4].
Tibæk et al. [4] studied total of 4,156 patients aged of 15 to 30 years old with first-ever stroke from 1994 to 2012, and stroke related hospitalizations increased from 11.97/100,000 personyears (PY) in 1994 to 16.77/100,000 PY in 2012.
The prevalence of PSD in young stroke patients
The after-effects of stroke can be severely debilitating and can prevent patients from returning to their previous lives. In addition to decreased functional ability, stroke can also deeply affect emotional and psychological health resulting in major anxiety and depression [8]. The prevalence of Post Stroke Depression is high, causing depressive symptoms in young patients almost 3 times more likely than older patients [9-11]. A more recent study done in 50 stroke survivors showed that symptoms of depression among individuals aged 27-36 years, 37–46 years, 47–56 years and 57–66 years were prevalent in 100%, 50%, 60%, and 29.63% of the population, respectively [12].
In 2013, PSD was evaluated for 6 months in 72 stroke patients aged 29-59 years who were attending a rehabilitation unit, and it was found that 67% were affected by depression [9]. Fourteen percent had borderline clinical depression, 34.7% had moderate depression, 15.2% had severe depression, and 2.9% had extreme depression [9]. Based on the results of this study, there is a significant correlation between depression and a decline in functional outcomes [9]. Young stroke patients are in the process of building their families, careers, and future. However, PSD halts these life processes and instead, backtracks them. Post-stroke depression is associated with decrease in quality of life, cognitive activity, and functional outcome [8,9,13]. Unfortunately, despite its devastating complications, PSD is often dismissed and 80% of the cases is inadequately managed by clinicians [14].
The effects of PSD in young patients
As previously stated, the consequences of stroke in young patients is significant because they are in the process of or at the peak of building their families, careers, and future [10]. Dealing with the devastating after-effects of stroke in addition to depressive symptoms can lead to a higher rate of morbidity and mortality [7,15-17]. Patients with depression have increase in functional impairments, social withdrawal, and cognitive disabilities compared to those without depression [8]. There is also a significant correlation between physical and intellectual limitations from stroke and difficulty in returning to work [18]. Physical ability is of great importance in men and women who are at their working age because they are often the main source of financial support for their families. Depression is one of the worst after-effects of stroke because it hinders the ability of young patients to go back to being independent and return to work [8,10]. Having a stroke at a young age can mean lifetime recovery after stroke [7]. Therefore, clinicians should be more sensitive in detecting young patients who are at risk of PSD and properly prevent or treat them to avoid further complications.
Methods
This paper used the Patient Intervention Comparator Outcome (PICO) framework to identify problem and to form the research question: “What is the current treatment for poststroke depression in young stroke survivors?” Key terms were then identified such as “young stroke” and “depression,” and used to search articles through online databases. Young stroke survivors with depression were taken as the population of the study. “Current treatment” was selected as the intervention. The comparison was with young stroke survivors who did not have depression. The desired outcome is to treat post-stroke depression in young patients.
Data extraction
The goal for data extraction was to find published articles relevant to the topic. Online database used to gather such studies included MedLine, PubMed, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Google Scholar. The key terms used to look for literature mentioned in this paper were “ young stroke, ” “ depression, ” and “ treatment. ” The compiled articles were then reviewed based on their pertinence to the topic. Reference lists of gathered studies were also analyzed to find relevant articles. This electronic database search was conducted in September through December 2019.
Literature selection
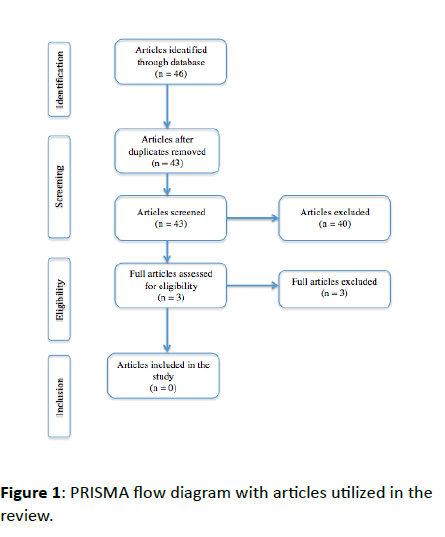
The PRISMA flow diagram was utilized for literature selection procedure (Figure 1). This search initially included 46 articles yielded from the online databases. After identifying 46 articles related to the topic, duplicate articles were excluded from the list. Studies were further excluded if they were not in English language, if the published year was below 2010, if stroke patients mentioned in the study had no depressive symptoms, and if the patient population was defined as younger than 18 year olds or older than 65 year olds. Lastly, the remaining articles were screened if they provided an answer to the research question formulated for this paper. In conclusion, no articles were identified that studied what the current treatment is for young stroke depression.
Results
Current treatment of PSD
Post stroke depression is prevalent in about 20 to 50% of stroke patients and it is a major cause of disability and mortality [16]. Significant risk factors for depression after a stroke include female gender, pre-existing mood disorder, younger age, motor or cognitive disability, low social support, single status, genetics, and neuroticism. Improving depressive symptoms have been correlated with better functional outcome, better quality of life, and better lifelong recovery and thus, a better chance of going back to work [17]. Available studies show that the most prevalent treatments for PSD are antidepressants such as selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants (TCAs) [19-21]. SSRIs and TCAs help with the recovery of both physical and cognitive function after a stroke by decreasing inflammation processes associated with depressive symptoms and as a result, they also increase survival up to 10 years after a stroke [15,22]. It is also known that antidepressants have high efficacy in improving independence, neurological impairment, and functional outcomes [23].
A 26-week study was conducted in four different stroke centers in Sweden, and patients who had depression after a stroke were given sertraline, an SSRI, or a placebo. By the end of 26 weeks, patients who received sertraline had a better quality of life and decreased hostility compared to the placebo group (p<.05) [24]. In their literature review, Xu et al. [21] reviewed 11 randomized control trials (RTCs), which assigned 740 stroke patients with depression to antidepressant or placebo treatment groups. This review found that there was a significant advantage in patients with antidepressants compared to the placebo group. Another study on randomized controlled trial was done on the efficacy of nortriptyline, a TCA, and fluoxetine, an SSRI, in both depressed and nondepressed stroke patients [15]. This trial also showed that antidepressants not only helped with depression, but also with patients ’ functional outcomes measured by modified Rankin Scale at one-year follow-up [15].
Other than pharmacological therapy, non-pharmacological approaches are also available to successfully treat PSD. Such approaches include cognitive behavioral therapy (CBT), electroconvulsive therapy (ECT) [19], ecosystem-focused therapy, acupressure, repetitive transcranial magnetic stimulation, exercise, music therapy, and light therapy among others [24-26]. These non-pharmacological approaches have also demonstrated improvements in PSD symptoms in stroke patients. Shen et al. [26] carried out a systematic review and meta-analysis of 22 randomized controlled trial studies, which included 1,764 patients and concluded that repetitive transcranial magnetic stimulation therapy was beneficial with positive findings in PSD patients.
Based on the literature, pharmacological therapy with SSRIs and TCAs have been highly successful and are superior to any other forms of treatment for post-stroke depression. However, no studies were found that address treatment options specifically for the young population. Although some practitioners are resistant to using SSRIs or TCAs due to their adverse effects, studies show that such adverse effects are more prominent in elderly patients. Therefore, more research is warranted to determine the effects of antidepressants on PSD specifically in younger patients.
Discussion
Major goals of treatment should not only be to reduce depressive symptoms but also to improve patients’ quality of life and regain functional ability so they can continue to build their career, family, and future for the remaining 40, 30, and 20 years. A successful outcome for elderly patients may be to reach independence in their activities of daily life. On the other hand, the goal for patients who are at their working age is to return to work and continue to build their lives. Therefore, there should be more aggressive approaches in treating depression in young patients.
When evaluating patients for their treatment plan, clinicians mainly focus on physical aspects of the after-effects of stroke. However, in addition to prescribing physical therapy, occupational therapy, and speech therapy, clinicians should recognize that implementing treatment for depression is equally, if not more important in young stroke patients. Just as occupation therapy, physical therapy, and speech therapy are almost immediately carried out as part of the stroke treatment plan, early detection of PSD and treatment implementation should be of utmost importance especially in young patients.
There are inconsistencies in what is the best treatment option for PSD in the general stroke population; most of the studies conclude that SSRIs and TCAs are the mainstay. The goal of this paper is to explore the current knowledge of treatment of PSD specifically in young patients. However, no studies were identified that specifically addressed this topic. The findings of this paper suggest that clinicians, nurses, therapists, and physicians ought to be more sensitive to the psychological needs of young stroke patients.
Stroke patients should be screened for depressive symptoms starting from acute phases of the disorder due to the high negative impact of PSD on the recovery. Special attention should be given to those who are young, and aggressive treatment with antidepressants or other alternative treatments should be implemented as soon as possible. In conjunction with medical treatment, psychological treatment should also be a priority in managing stroke patients during the acute phase.
Conclusion
Neurologists and nurses play a crucial role in helping young stroke patients to recover, restore, and possibly resume their previous lives. By being sensitive and knowledgeable in treating PSD in young patients, clinicians can further help patients to recover physically, socially, and psychologically. Currently, there are no treatment guidelines that specifically target PSD in young stroke patients. Although there are few treatment options for PSD in general, further research is warranted to evaluate the effects of current PSD treatment options that specifically target the young stroke population.
References
- Stroke ND (2019) National Heart, Lung, and Blood Institute. Retrieved November 13, USA.
- Benjamin EJ, Muntner P, Alonso A (2019) Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation 139: 56-528.
- Ramirez L, Kim‐Tenser MA, Sanossian N, Cen S, Wen G, et al. (2016) Trends in acute ischemic stroke hospitalizations in the United States. J Am Heart Assoc 5: e003233.
- Tibæk M, Dehlendorff C, Jørgensen HS, Forchhammer HB, Johnsen SP, et al. (2016). Increasing incidence of hospitalization for stroke and transient ischemic attack in young adults: A registry‐based study. J Am Heart Assoc 4: e003158.
- Smajlovic D (2015) Strokes in young adults: Epidemiology and prevention. Vasc Health Risk Manag 11: 157-164
- Fox C (2019) Ischemic stroke in children and young adults: Epidemiology, etiology and risk factors. In: Dashe JF (ed), UpToDate. Retrieved November 15.
- Ekker MS, Boot EM, Singhal AB, Tan KS, Debette S, et al. (2018) Epidemiology, aetiology, and management of ischaemic stroke in young adults. The Lancet Neurology 17: 790-801.
- Dar SK, Venigalla H, Khan AM, Ahmed R, Mekala HM, et al. (2017) Post stroke depression frequently overlooked, undiagnosed, untreated. Neuropsychiatry 7: 906-919.
- Amaricai E, Poenaru DV (2016) The post-stroke depression and its impact on functioning in young and adult stroke patients of a rehabilitation unit. Retrieved November 13, 2019 J Ment Health 25: 137-41.
- Kapoor A, Si K, Yu AY, Lanctot KL, Herrmann N, et al. (2019) Younger age and depressive symptoms predict high risk of generalized anxiety after stroke and transient ischemic attack. Stroke 50: 2359-2363.
- Srivastava A, Taly A, Gupta A, Murali T (2010) Post-stroke depression: Prevalence and relationship with disability in chronic stroke survivors. Ann Indian Acad Neurol 13: 123-127.
- Ibeneme SC, Nwosu A, Anyachukwu CC, IbenemeGC, Bakare MO, et al. (2017) Burden and factors associated with post-stroke depression in East central Nigeria. African Health Sciences 17: 859.
- Ji-hua Xu (2018) Efficacy of escitalopram oxalate for patients with post-stroke depression. Medicine 97: 1-3.
- Lokk (2010) Management of depression in elderly stroke patients. Neuropsychiatr Dis Treat 6: 539-549.
- Robinson RG, Jorge RE (2016) Post-stroke depression: A review. Am J Psychiat 173: 221-231.
- Brigadeiro D, Nunes J, Gil TV, Costa P (2017) Poststroke depression. European Psychiatry 41: S524-S525.
- Towfighi A, Ovbiagele B, El Husseini N, Hackett ML, Jorge RE, et al. (2017) Poststroke depression: A scientific statement for healthcare professionals From the American Heart Association/American Stroke Association. Stroke 48: e30–e43.
- Balasooriya-Smeekens C, Bateman A, Mant J, Simoni AD (2016) Barriers and facilitators to staying in work after stroke: Insight from an online forum. BMJ Open 6: e009974.
- Pompili M, Venturini P, Lamis DA, Giordano G, Serafini G, et al. (2015) Suicide in stroke survivors: Epidemiology and prevention. Drugs & Aging 32: 21-29.
- Dwyer Hollender K (2014) Screening, diagnosis, and treatment of post-stroke depression. J Neurosci Nurs, 46: 135-141.
- Xu X, Zou D, Shen L, Liu Y, Zhou X, et al. (2016) Efficacy and feasibility of antidepressant treatment in patients with post-stroke depression. Medicine 95: e5349.
- Villa RF, Ferrari F, Moretti A (2018) Post-stroke depression: Mechanisms and pharmacological treatment. Pharmacol Ther 184: 131-144.
- Mead GE, Hsieh CF, Lee R, Kutlubaev MA, Claxton A, et al. (2012) Selective serotonin reuptake inhibitors (SSRIs) for stroke recovery. Cochrane Database Syst Rev 11: CD009286.
- Murray V, von Arbin M, Bartfai A, Berggren AL, Landtblom AM, et al. (2005) Double-blind comparison of sertraline and placebo in stroke patients with minor depression and less severe major depression. J Clin Psychiatry 66: 708-716.
- Hadidi NN, Huna Wagner RL, Lindquist R (2017). Nonpharmacological treatments for post-stroke depression: an integrative review of the literature. Res Gerontol Nurs 10: 182-195.
- Shen X, Liu M, Cheng Y, Jia C, Pan X, et al. (2017) Repetitive transcranial magnetic stimulation for the treatment of post-stroke depression: A systematic review and meta-analysis of randomized controlled clinical trials. J Affect Disord, 211: 65-74.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences